Biomaterial scaffolds containing extracellular vesicles from stem cells to control and promote heart muscle repair after heart attack

Scientists of the ICREC group at the Germans Trias i Pujol Research institute (IGTP) continue to refine their technology for repairing cardiac tissue after a heart attack. In a paper published in Bioactive Materials they present their latest work in which they use implanted scaffolds containing no cells, but extracellular vesicles that promote the repair of myocardium damaged in a heart attack.
The ICREC group at the Germans Trias i Pujol Research institute (IGTP), led by Dr Antoni Bayes-Genis has extensive experience in research into heart repair technology and have an ongoing clinical trial to repair the damaged heart with an artificial implant containing stem cells (PeriCord), licensed in 2018 by the Spanish Agency for Medicines and Medical Products (AEMPS). The group is continuing to investigate the mechanisms by which stem cells can help restore damaged heart muscles. Their latest research published in Bioactive Materials has further perfected the tissue engineering design and they have shown that the heart muscle can be induced to regenerate through the application of extracellular vesicles (EV) in a bioimplant, without the addition of actual cells.
"Heart muscle is damaged in a myocardial infarction (heart attack)," explains Dr Marta Monguió-Tortajada, one of the lead authors of the new paper. "Immune cells rushing to clear the injured area are necessary in the beginning, but can also cause uncontrolled inflammation and further damage." If a large area of the heart is scarred and cannot beat properly, the patient might lately suffer heart failure, a chronic condition for which the only current treatment to completely restore the cardiac function is a heart transplant; a traumatic operation. Additionally, with the rise of heart disease in the modern world, healthy heart donations are hard to come by." A far better way is to use advanced therapies so the patient can regenerate their own heart tissue," Dr Santiago Roura, co-author of the study continues, "But this requires an intricate understanding of all the processes involved, and this is where our work comes in."
The group has previously shown how stem cells introduced through a bioimplant can reduce the damaging immune response. "One of the big issues with this technology is that so far we have seen very few cells moving from the implant into the host's muscle tissue," says Dr Cristina Prat-Vidal, also a lead author and leading the PeriCord project. "This could indicate that stem cells can trigger tissue repair through other mechanisms than themselves, such as extracellular vesicles," she adds.
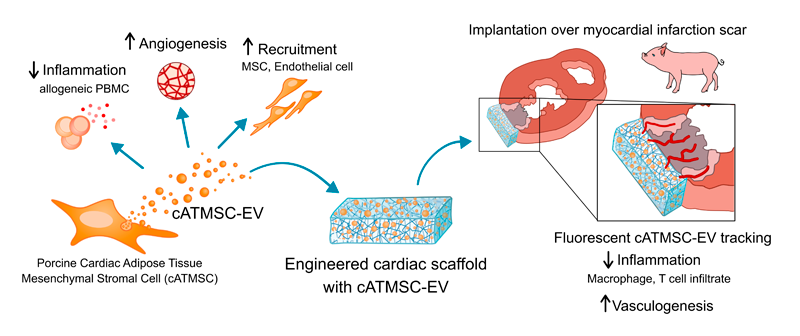
Now working together with the REMAR-IVECAT group led by Dr Francesc E. Borràs, also at the IGTP, the researchers have separated out extracellular vesicles (EV), tiny particles that pinch off from a cell and carry many substances that cells use to communicate with each other. "We have used a technology called size exclusion chromatography (SEC), to purify these EV and we have introduced them into a scaffold made of biological structural material but with all the previously existing cells removed," says Monguió-Tortajada. The EVs are fixed into a hydrogel and introduced into the scaffold, making up the bioimplant that is applied to damaged heart tissue, "it acts like a bioactive band-aid", Monguió-Tortajada adds. In the laboratory, the group have observed the EVs working in two ways: they stop inflammation; and additionally, they recruit cells that can repair the heart muscle and encourage the growth of blood vessels, something which is vital if heart muscle is to be able to function properly.
Researchers then added the bioimplants to damaged heart muscle in a pig heart attack model, a procedure performed by Dr Carolina Gálvez-Montón. The scaffolds successfully integrated with the cardiac tissue and the EVs were seen to have moved to the damaged tissue, where they increased the growth of cells forming blood vessels and reduced the entry of the immune cells that can cause further damage.
"This is an exciting result" Monguió-Tortajada tells us. "While we still have to see if it induces a benefit in cardiac function, for which the pig model is very helpful, it is a possible treatment for heart attack that introduces no foreign cells to the body, avoiding the rejection risks of such treatment. The implantation of EVs from stem cells harnesses a signaling system of the body's own cells to calm the immune system and reduce inflammation, while at the same time calling in cells that can repair cardiac muscle and encourage the regrowth of blood vessels. Additionally, with this approach we can control the position and dosage of EVs extremely precisely to provide a highly-controlled environment for heart tissue regeneration."
The study has been possible thanks to the collaboration with Dr Anna Rosell's group at Vall d'Hebron Research Institute (VHIR, Barcelona) and Dr Miguel Ángel Ramírez's group at Instituto Nacional de Investigación en Tecnología Agraria y Alimentaria (INIA, Madrid).
This work has been funded by the Fundació la Marató de TV3, the Instituto de Salud Carlos III from the Ministry of Health and also the Ministry of Economy and Competitiveness (MCINN) in Spain and the European Commission Regional Development Funds. Both ICREC and -REMAR-IVECAT are consolidated groups with funding from the Agency for Management of University and Research Grants (AGAUR) of the Government of Catalonia, which also supplied a PERIS grant. ICREC is part of both the CIBER Cardiovascular and Spanish Cell Therapy (TerCel) networks.
Original paper
Local administration of porcine immunomodulatory, chemotactic and angiogenic extracellular vesicles using engineered cardiac scaffolds for myocardial infarction
Monguió-Tortajada et al. Bioactive Materials, Volume 6, Issue 10, October 2021, Pages 3314-3327 doi:10.1016/j.bioactmat.2021.02.026
